View The Detail’s ambulance response interactive map in a full screen map
By Kathryn Torney
WHERE you live in Northern Ireland makes a massive difference to ambulance response times in life threatening situations, it can be revealed today.
An investigation by The Detail has uncovered a disturbing postcode lottery when it comes to ambulance service response times.
We analysed 215,349 emergency calls made to the Northern Ireland Ambulance Service (NIAS) during 2010 and 2011 and found a wide variation in response times in different postcode districts.
Among the very long waits experienced by a minority of patients, a person suffering from stab/gunshot/penetrating trauma injuries had to wait over 46 minutes for the ambulance service to arrive on the scene.
We have published an interactive map showing the response times for each postcode district in Northern Ireland during 2010 and 2011 and also the longest Category A call wait for an ambulance in each area. Category A are the calls considered life threatening.
And we have compiled tables to show all Category A calls with a response time of over an hour and all Category B calls (serious but not life threatening) with a response time of over an hour and a half. Click here to see these tables.
For Category B cases, patients should receive a response within 21 minutes in 95% of cases.
From April 2011, the Northern Ireland target is that an average of 72.5% of Category A calls should be responded to within eight minutes – and not less than 65% in any health trust area.
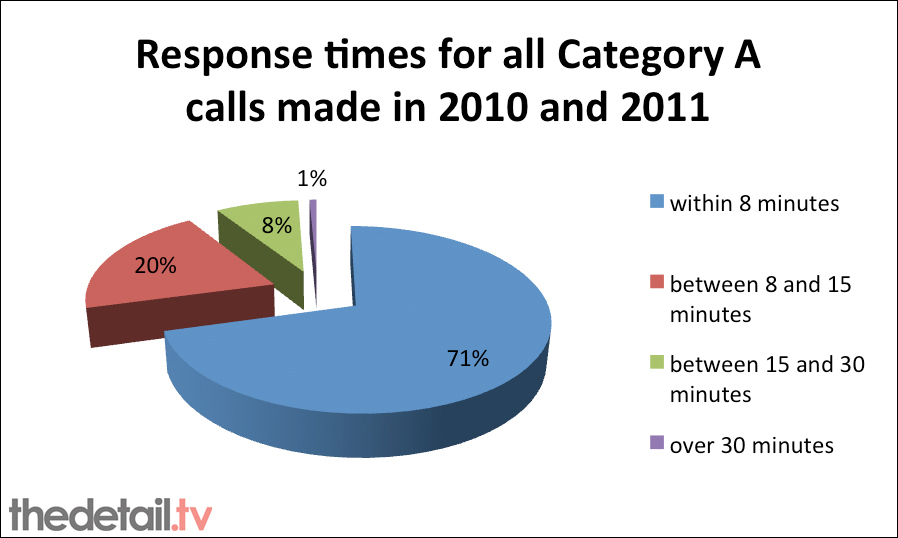
An ambulance or rapid response vehicle (RRV) arrived within eight minutes for 71% of the 88,865 Category A calls made during 2010 and 2011.
However, in 12 of the 80 postcode districts only 10% or less of all 999 Category A calls made within each district were responded to within the key target of eight minutes.
The figure was just 3% in the Clogher area (BT76) – compared to 91% in central Belfast’s BT12 area. Some of the lowest rates were in Fermanagh and parts of Co Tyrone.
Response times are based on the arrival of either an ambulance or rapid response vehicle (RRV) at the scene.
In a detailed response to The Detail’s findings, NIAS chief executive Liam McIvor said: “The Northern Ireland Ambulance Service will continue to identify and develop measures to provide the best possible ambulance care to all patients, particularly in those areas which are difficult to reach within our eight minute response target.”
After our story was first published (on March 11th), the chair of Stormont’s health committee released a statement to say that members would be meeting with the Ambulance Service Control Room to examine what could be done to improve response times in rural area.
The chair, Sinn Fein’s Sue Ramsey, said: "The recent report highlighting the longer call out times for ambulances in rural areas is concerning.
“What we need is an approach bringing targeted investment to get these arrival times up to speed. Many are too close to the ‘golden hour’ of emergency services delivery.
“As such the health committee will be meeting with the Ambulance Service Control Room in a number of weeks as part of the process examining what can be done to improve these times.”
And our figures have also featured in an article on The Guardian newspaper’s Datablog.
INCREASING PRESSURE
The ambulance wait figures are further evidence of serious pressures within Northern Ireland’s health system following the closure of a number of accident and emergency units.
Earlier this week, the Royal College of Nursing said reports of seriously long trolley waits for patients and hospital staff being at breaking point were “totally unacceptable”.
The increasing pressure on the remaining acute hospitals in Northern Ireland is one factor influencing ambulance response times. Many patients have to spend longer travelling in ambulances getting to hospitals from rural areas.
There can also be serious delays in handover when ambulances finally reach hospitals with patients.
While extremely long waits were rare among the tens of thousands of overall calls made during 2010 and 2011, some individual cases logged by the NIAS system make alarming reading.
There was a one hour 29 minute wait for someone thought to be having a stroke in the Cookstown area. This was in December 2010 so the response time may have been influenced by the heavy snow experienced across Northern Ireland that month.
Other long waits for patients in life threatening conditions include:
• Over 46 minutes for stab/gunshot/penetrating trauma incident in BT44 (Cushendall area) in December 2011.
• A 45 minute wait for an ambulance following an assault/sexual assault in BT64 (Craigavon area) in April 2010.
• A 52 minute wait for someone with breathing problems in May 2011 also in the BT44 area.
• In July 2010, a patient waited for 43 minutes in Larne area (BT40). This call was logged in the pregnancy/childbirth/miscarriage category.
The longest wait for a life threatening Category A call response was recorded as two hours 50 minutes – for a drowning/diving/scuba accident in Irvinestown. However, a spokesman for the NIAS said the crew were at the scene much earlier waiting for the casualty to be located and brought to land by search and rescue teams. It is therefore thought that the “arrival at scene” time was not recorded correctly.
The NIAS also said that the timing for a recorded two hour 10 minute wait for a cardiac patient in Armagh had been entered incorrectly manually.
There was however a three hour 10 minute wait for a Category B call logged as a “fall” in July 2011 in BT15 in the Greater Belfast area.
THE FIGURES
The Northern Ireland Ambulance Service publishes response times on a Northern Ireland-wide and health trust basis – but does not routinely publish statistics at postcode district level.
Using Freedom of Information legislation, we requested a breakdown of information on all Category A and B emergency calls made to the Northern Ireland Ambulance Service during 2010 and 2011.
Category A calls are those 999 calls where there is an immediate threat to life while Category B are incidents considered serious but not life threatening.
The NIAS provided us with a large dataset of information on each of the 215,349 calls including:
• the time it took for an ambulance or rapid response vehicle (RRV) to arrive.
• the postcode district.
• the chief complaint/symptom.
• the month and year the call was made.
• which health trust the emergency call originated from.
We also asked how many people connected to each call out had died but this information could not be provided.
An ambulance or rapid response vehicle (RRV) arrived within eight minutes for 71% of the 88,865 Category A calls, 20% between eight and 15 minutes, 8% between 15 and 30 minutes and 439 responses (1%) took longer than 30 minutes.
Of the total 126,484 Category B calls (serious but not life threatening) made in 2010 and 2011, almost 93% were responded to within the target of 21 minutes or less.
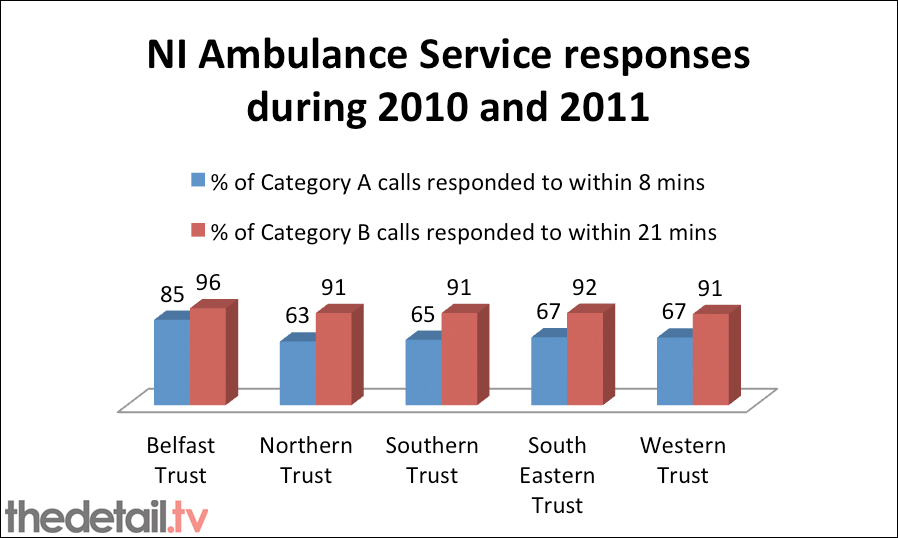
However, there were major differences between responses in different health trust areas – for example 85% of Category A calls in the Belfast Trust area were responded to within eight minutes, compared to 63% in the Northern Trust area.
Response times to incidents in December 2010/January 2011 may have been affected by the heavy snow afflicting much of Northern Ireland during that period. However, in other cases, the cause of serious delays is unclear.
Just over 4,120 of the Category A calls were recorded as being answered within less than a minute. The NIAS said this is because the performance time begins to be calculated only when the location and chief complaint of the patient has been received from the emergency caller. By then, an ambulance may already be on its way.
THE HOSPITAL CAMPAIGNER’S VIEW
Save The Mid was established as a campaign group in May 2010 to lobby for acute health services in the mid Ulster area.
The group’s spokeman Hugh McCloy said that the removal of acute inpatients services from some hospitals had left people living outside key urban areas at great risk.
He said: “There was an expectation that the Ambulance Service would fill the gap created by removing acute services from areas like Mid Ulster.
“How could those in a decision making position ever think that an ambulance could fill the 700 square mile void of acute services left in central rural Northern Ireland after the removal of the accident and emergency departments in Mid Ulster, Dungannon and Omagh hospitals?
“Politicians and health chiefs can celebrate and discuss what services a local hospital will provide rural communities in terms of outreach and outpatient care but do these services save lives? The simple answer is no.
“The reality is that there is a lack of capacity in accident and emergency units and in hospital wards. This holds up ambulances at hospital entries. Tracking systems installed within ambulances can also leave rural areas devoid of ambulance cover when ambulances are routed and kept in urban areas.
“The role of an emergency service is to save lives but A&E wards are left looking more like waiting rooms and now we see that response times for ambulances are very poor in some postcode districts. All of this puts patients’ lives at risk.”
“IT IS DIFFICULT TO PROVIDE AMBULANCE SERVICES IN RURAL AREAS”
We posed a series of questions to Health Minister Edwin Poots based on our findings and he gave a detailed reply.
However, he did not respond to us asking if it was acceptable to have a “postcode lottery” for ambulance response times or whether or not the situation was likely to get worse due to financial cutbacks and increasing demands on the health service.
The Minister said the Northern Ireland Ambulance Service strives to ensure all Category A calls are responded to as quickly as possible and within target irrespective of incident location.
“Rural areas are more difficult to provide ambulance services for because of their topography and sparse populations,” he said. “As a result, the department has been working with NIAS for many years to improve ambulance response times in rural areas.
“Additional deployment points have been provided, along with additional rapid response vehicles (RRVs), new information and dispatch systems and state-of-the-art vehicle location and satellite navigation systems.
“The Regional Emergency Medical Dispatch Centre also now hosts doctors who triage the calls that come in, making sure that A&E ambulances and RRVs are sent only to appropriate emergency incidents and to provide alternatives as required.”
Almost £100m is being spent between 2008 and 2018 to modernise the Northern Ireland Ambulance Service and replace its fleet and equipment on a regular basis.
Mr Poots continued: “Given the lower level of Category A demand in rural areas it would not be operationally or financially feasible to deploy an emergency resource in areas where demand indicates it will sit unused for significant periods of time.
“NIAS deploys ambulances tactically to ensure that available ambulance resources are deployed where calls are most likely to originate and where existing ambulance resources can have the greatest impact for the greatest number of patients.
“This means that the response to an emergency call may be provided by an ambulance or RRV which is not actually based at the nearest ambulance station.”
Mr Poots added that, unlike other ambulance services in the UK, all ambulances and RRVs are routinely crewed by staff who are paramedics.
He concluded by criticising people who call 999 for help with non-emergencies. This was the case for one in five 999 calls for an ambulance last year. The Ambulance Service received 1,686 hoax calls, 2,476 people called for information only and 735 people called for help to get them back into bed.
The Minister warned: “This is a waste and is putting the lives of those in real need at serious risk.”